Porcelain, gold, or tooth-colored resin inlays and onlays offer a minimally invasive way to restore damaged smiles when teeth are too compromised for basic fillings but not bad enough for crowns. Crafted via digital impressions to seamlessly fit fractured, decayed or cracked teeth, these partial yet durable restorations rebuild structure and confidence.
What are inlays and onlays?
Think of inlays and onlays like precision-fit mini tooth implants. When you chip or crack a tooth down to the nerves, instead of drilling out healthy areas for a cumbersome crown, these conservative restorations save the day!

An expert dentist first scans the unique cavity or missing chunk area with advanced imaging tools. Next, a dental technician hand-crafts a customized inlay or onlay designed to flawlessly integrate into the gap or fracture using biocompatible porcelain, resin, or gold.
Within a week or two, the meticulously shaped restoration arrives to be bonded into place for a natural and structurally sound fix. Both inlays and the larger onlays used for more substantial chewing surface damage conserve healthy tooth structure and function beautifully.
Materials used to build inlays and onlays

- Porcelain: With its tooth-like luster and durability, porcelain is a go-to for natural-looking inlay restorations that blend beautifully. Skillful dental ceramists can even mimic subtle shade variations just like real enamel!
- Gold: Believe it or not, gold makes a versatile inlay building block – biocompatible, strong yet flexible, and less abrasive than porcelain on opposing teeth during chewing. And it lasts decades despite wear and tear! Only downsides? Price and aesthetics.
- Composite resin: For a budget-friendly alternative, dental laboratories craft custom inlays from plastic/glass blended composite resin. While less robust than porcelain and gold, composite resins can match neighboring tooth tones well.
- Glass ionomer cement: This acrylic/glass mixture offers another cost-effective inlay route that can closely match natural dentin hues. However, glass ionomer cements tend to lack the durability and longevity of other materials for extensive repairs.
Choosing the optimal material comes down to striking the right balance between strength, resilience, aesthetics and affordability. Discuss personalized pros and cons with your restoration dentist when considering inlays and onlays!
What are the indications for inlays and onlays
While inlays and onlays artfully restore fractured or decayed smiles, they serve best in specific situations depending on the tooth defects involved.

Some specific indications for inlays and onlays include:
- Repairing mild to moderate areas of tooth decay: When destruction is too substantial for a basic filling but not severe enough for a onlay or full crown, inlays offer durable intermediary restoration contouring to the unique cavity shape.
- Restoring severely damaged teeth: Significant cracks, fractures, or gaps involving the biting surface demand reinforcement wider than inlays can provide. This is where sturdy onlays bond flawlessly into more considerable defects.
- Strengthening and reinforcing a tooth: Whether used for sizable crevices caused by trauma or moderate decay near the nerve, inlays and onlays durably shore up structural weakness vulnerable in regular fillings.
- Improving the appearance of a tooth: Unlike metal amalgam fillings, porcelain and composite inlays/onlays blend attractively with surrounding tooth color. They maintain a beautifully natural look in visible areas like a front cracked incisor.
In a nutshell, inlays and onlays strike an ideal balance between strength, resilience, and precision integration for particular types of oral defects compared to other options.
The process of building inlays and onlays
Preparation
Transforming the tooth into a blank canvas marks the first step in inlay and onlay creation. Using specialized instruments, the dentist removes decay and damaged areas, reshaping the remaining tooth structure into a stable foundation. Retentive features like slight undercuts strengthen adhesion while conservative walls limit unnecessary tissue removal. The preparation balances durability and preservation.
Impressions
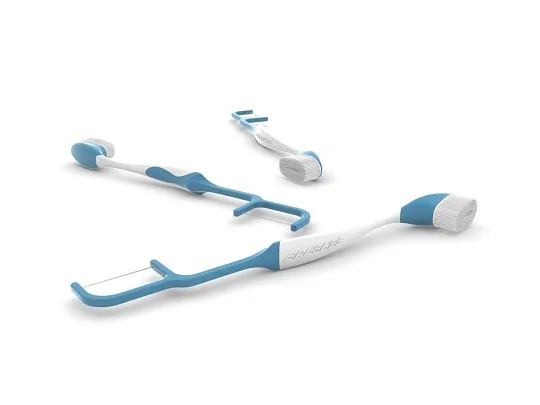
With the preparation finished, the tooth’s contours are imprinted in detailed molds. Analog impressions record intricate anatomical details in putty which then gets poured in stone. Digital scanners use advanced optics and software to capture hyperrealistic 3D maps of the preparation. These guides provide the inputs for designing anatomically accurate restorations.
Fabrication

Inlays and onlays take shape from either blocks of ceramic or lost-wax casted metals. In ceramics, computer-guided milling machines carve intricate anatomy from porcelain blanks. In gold restorations, technicians invest in the wax pattern and then burn away the wax to replace it with casted gold. Margins are carefully perfected to ensure smooth, seamless transitions between tooth and restoration.
Bonding
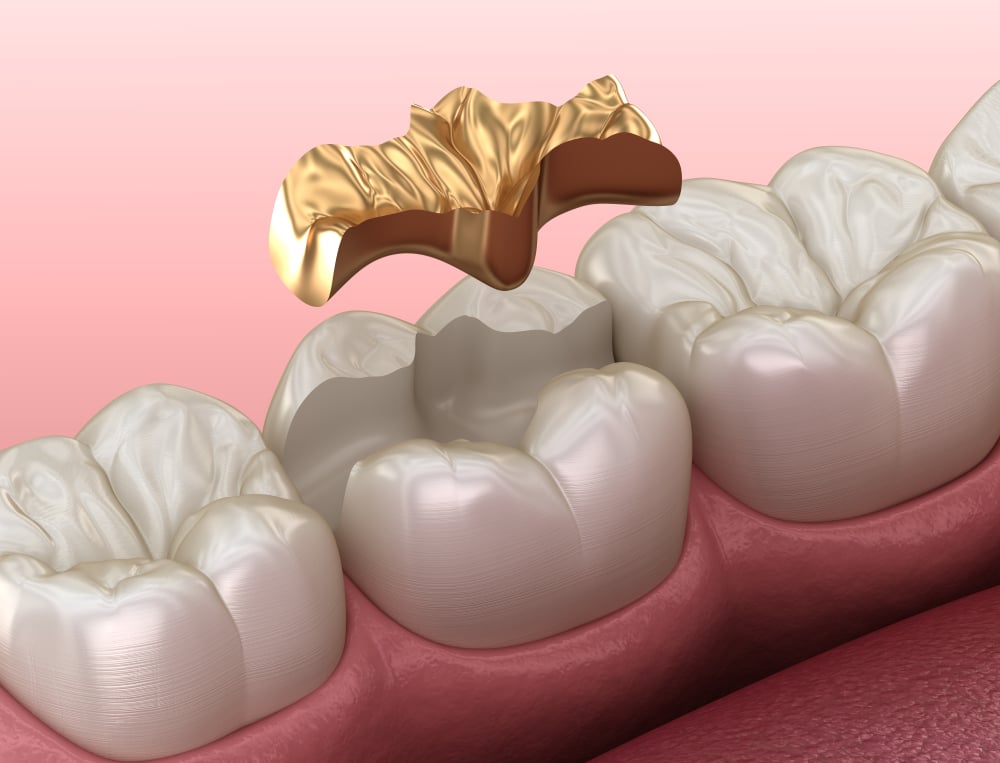
The moment of truth – will the onlay fit precisely into place? Proper marginal seals and occlusion mean success, and bonding agents and cements permanently fix the restoration. Light curing and excess removal finish the process, blending the inlay or onlay seamlessly with the surrounding tooth structure. Form and function are beautifully restored.
Follow-Up
While previous steps demand technical prowess, follow-ups focus on patients’ needs. Do temperatures trigger sensitivity? Can patients comfortably chew across the full range of motion? Dentists fine-tune contacts or occlusion and smooth any rough areas. Just as importantly, they provide reassurance about the restoration’s performance and longevity. Follow-ups optimize outcomes and build patient confidence.
Comparing traditional impressions with digital scanners
Dentistry unquestionably progresses toward digitization, yet traditional impression methods still play an important role – at least for now. Like the gradual adoption of digital photography, budget, expertise, and preferences inform practices’ choices between intraoral scanners and conventional impression materials. Identifying the strengths and limitations of both guides teams transitioning towards optimal workflows.

For over a century, dentists mixed rigid alginate or molded silicone putties and loaded tray after tray to capture oral anatomy. Technique and timing determined success as teams raced to set materials before distorting changes. Missteps marred intricate details or dimensional precision critical for treatments like crowns or aligners. Mastering these manual steps defined dentistry’s past, but left little tolerance for error.
Alternatively, graceful wand-shaped intraoral scanners project structured light patterns while advanced optics and AI translate reflections into 3D models. On-screen, dentitions emerge in vibrant living color with impressive accuracy and speed. Reducing human variability in capture, digital scans excel in precision-dependent procedures. Yet economic barriers slow mass adoption. While digital scans mesmerize with their crisp precision, economic factors still favor conventional impressions for some practices. Scanner units require capital investments from five to over one hundred thousand dollars – no small fee for smaller practices. Moreover, without advanced training and troubleshooting skills, incorporating these devices slows instead of expedites treatment. Practitioners comfortable with putties and trays leverage existing infrastructure and expertise to deliver care relying on proven techniques.
Cost certainly impacts technology integration, especially for smaller practices. All-in-one scanner units range from $5,000 to $150,000 – no small tickets for lean budgets more comfortable with proven impressions. Moreover, digital workflows demand advanced troubleshooting skills and training investments to realize efficiency gains. Thus, those mastering traditional techniques stick to their impression materials to deliver quality carePatients notice little difference between intraoral camera wands or loaded impression trays. So rather than pitting digital against traditional, selecting modalities based on budgets and expertise makes implementation steady and practical. Workflows evolve one practice at a time.
What is the cost of an inlay or onlay?
Getting quoted a price between $500 and $1500 for a single inlay or onlay restoration may initially give some patients sticker shock. However, considering these tooth-colored treatments’ longevity and protection of surrounding healthy tooth structure helps justify costs exceeding traditional fillings. Understanding exactly what influences the investment in inlays and onlays empowers patients to budget accordingly.
Since inlays and onlays must withstand extreme pressures concentrated along the chewing surface, durability matters. Durable materials and labor-intensive fabrication ramp up expenses. Skilled ceramists craft glass-based porcelain or composite resin blocking to ensure lifelike aesthetics. In other cases, milling machines carve restorations from single blocks under precise digital control. For gold inlays and onlays, complex lost-wax casting methods allow intricate margins and contacts. Throughout the workflow, technicians’ expertise factors into the final tab.
The tooth’s location also tweaks quotes up or down. Larger molars span more chewing real estate and require more material compared to incisors and bicuspids. Additionally, the artistry needed for visible smile zone restorations ensures seamless color blending with surrounding teeth. Simpler cases mean simpler pricing.
Geography plays perhaps the most unpredictable role in cost variation because overhead expenses differ significantly across regions. Rural solo practitioners likely charge less than big-name studios in metropolitan hubs. Offshore dental tourism hotspots cater to bargain hunters too. Yet reduced price tags often reflect lower margins rather than sheer generosity. Researching local rates provides a realistic context.
While inlays and onlays demand more upfront investment than direct fillings, choosing quality materials and technical mastery pays long-term dividends in function and aesthetics. Understanding cost breakdowns helps patients budget wisely as they safeguard oral health.